Why Shifa Piles Clinic?
We Offer quality Ayurvedic treatment in a modern specific way by following Ayurvedic principles, and traditional methods which have the highest success rate and with no recurrence chances in one lifetime.
We Offer quality Ayurvedic treatment in a modern specific way by following Ayurvedic principles, and traditional methods which have the highest success rate and with no recurrence chances in one lifetime.
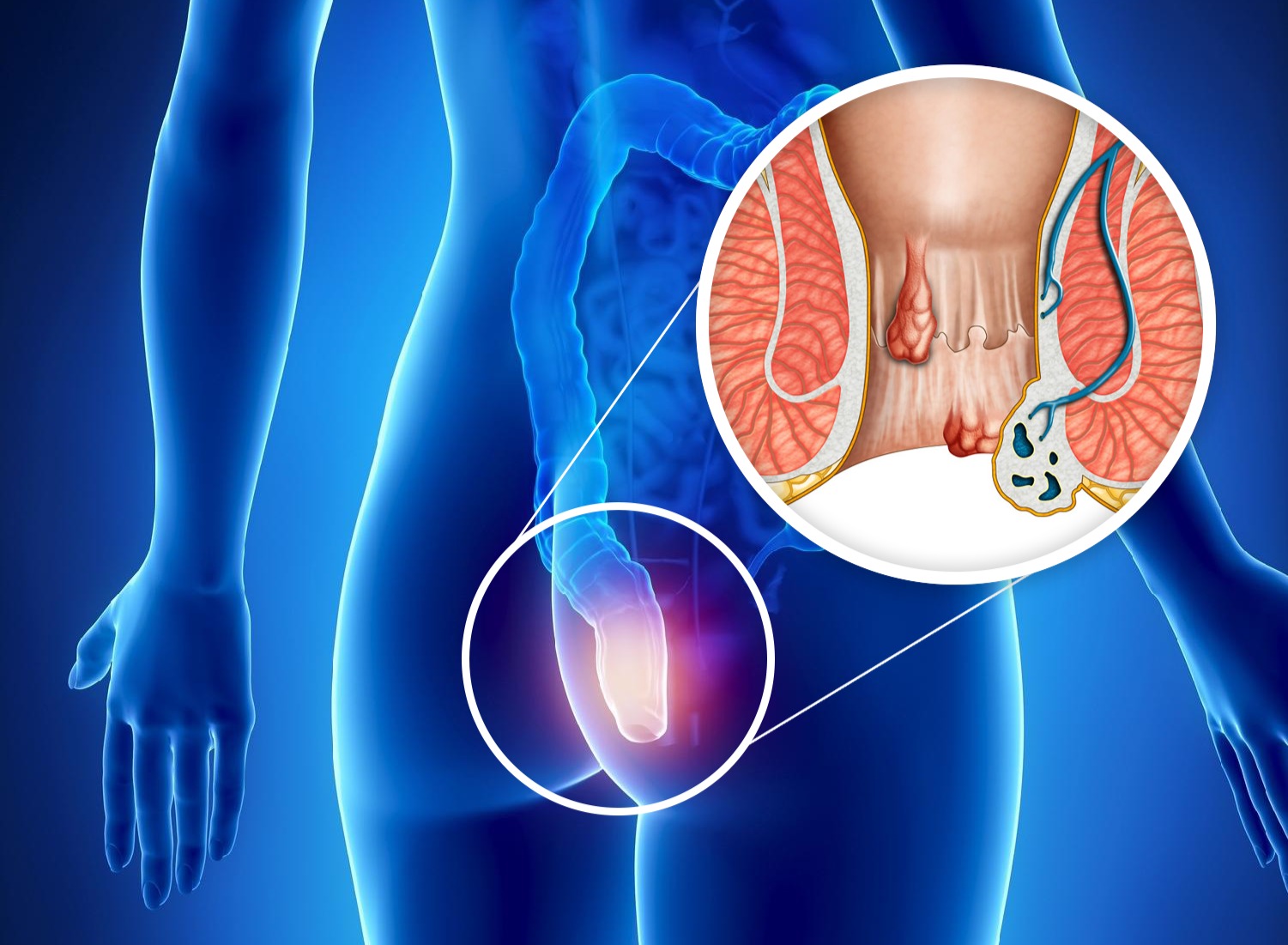
Piles / Hemorrhoids, is a very common anorectal condition. Piles are collections of veins and tissues located at the anal area that becomes swollen and inflamed. Piles may develop around the anal skin or inside the rectum. Piles is common in the case of both men and women.
Know MoreAn anal fistula is a tunnel that runs from the anal opening and connects the skin around it. An anal fistula mostly forms after an infection that did not heal properly. In human anatomy, the external opening through which feces are expelled is known as the anus.
Know MoreAn anal fissure is a tear or cuts in the thin lining of your anus that exposes the muscle around which is called the anal sphincter. The damage in the skin can often pull apart the edges of the fissure, cause the muscle to spasm, and make the condition worsen.
Know MoreWith our No Cost EMI option, you have one less thing to worry about health. Every patient can now avoid lump sum payments on medical bills of surgeries with the No Cost EMI option.
It just takes 30 - 45 minutes for procedure. Patient discharge around 6 hours after the surgery from our clinic.
Female Surgeons are also available to treat Piles, Anal Fistula, Anal Fissure, Pilonidal Sinus.
Treatements are done using most advanced technology. You will be able to Join work in 2 - 3 days.
We offer free follow-up consultations and instructions including dietary tips as well as exercises to every patient to ensure they have a smooth recovery to their daily routines.
Low Surgery Cost
ZERO % Reoccurrence
Low Blood Loss
Quick Recovery
Minimal Cuts
Minimal Scars and Stiches
At Shifa Piles Clinic we have successfully treated many complex piles problems that patients is suffering from, enabling them to get back to a happy life.
Doctors
Cities
Happy Patients
Successful Operations
Don't Let Piles Ruin Your Day!
Get Ayurvedic Treatment with no Side Effects
Everything You Need To Know About Piles
Piles or hemorrhoids, is a very common anorectal condition. Piles are collections of veins and tissues located at the anal area that becomes swollen and inflamed. Piles may develop around the anal skin or inside the rectum. Piles is common in the case of both men and women.
If global medical reports are to be believed, one out of every four adults suffers from piles or hemorrhoids at some or other point in their life. Piles is most common in people within the age group of 50-60 years but can affect people of other age groups too. No medical expert to date could ascertain the exact cause of hemorrhoids. However, several risk factors have been identified which can significantly increase an individual’s chances of developing piles. Piles can be managed with home remedies to a certain extent at an initial stage, but when piles grow severe or become advanced, medical intervention is extremely important.
The condition of piles is formed by constant pressure in the lower rectum. When a person constantly exerts pressure in areas around his rectum and the anus, due to reasons like constipation or lifting heavy weights, the blood vessels around those parts bulge and become swollen, forming piles.
Due to constant straining, sometimes the veins might get wider and engorged with more blood than usual. These veins might form into one or more piles.

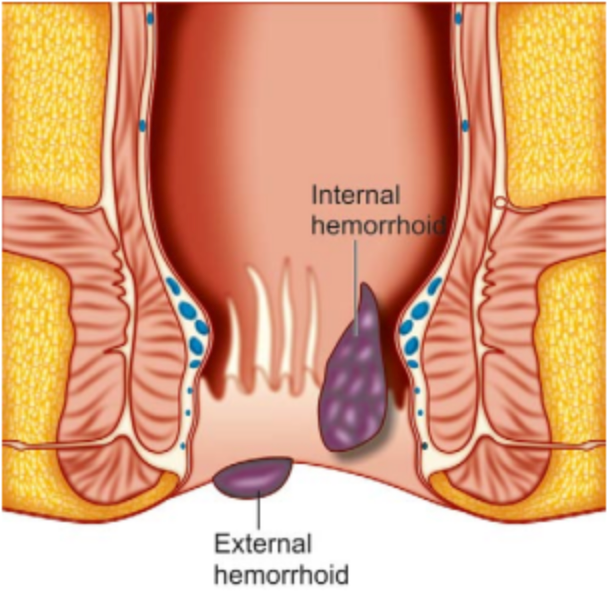
Hemorrhoids are classified based on the ‘Dentate line’
Hemorrhoids that originate distal to the dentate line and are lined with modified squamous epithelium are called External Hemorrhoids
Hemorrhoids that originate proximal to the dentate line and are covered with mucosa are called Internal Hemorrhoids
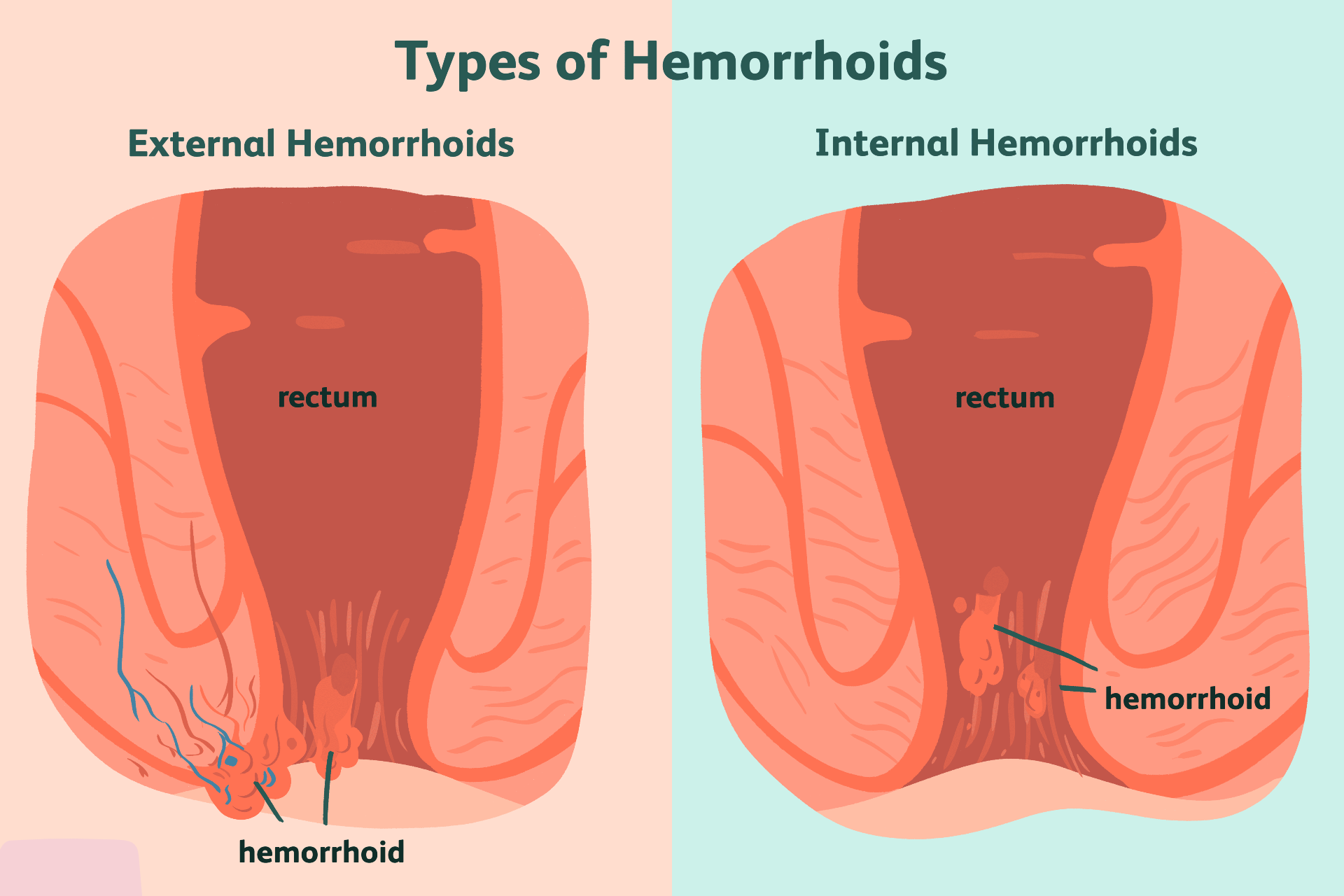
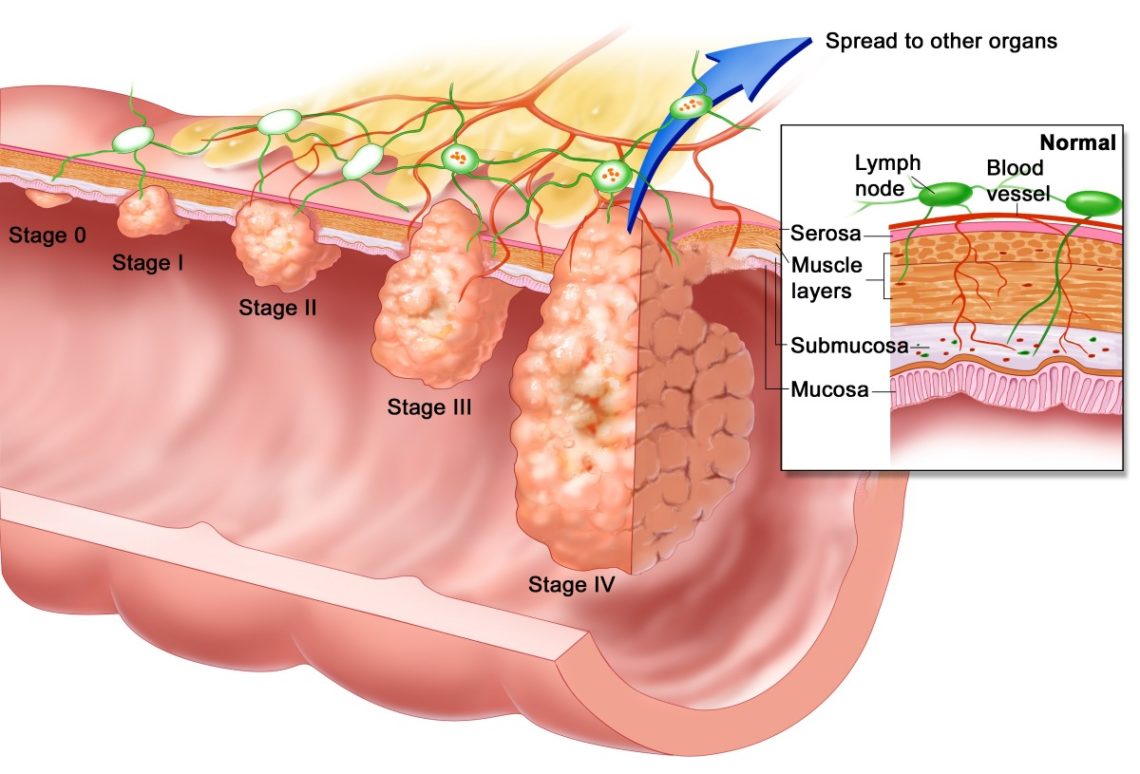
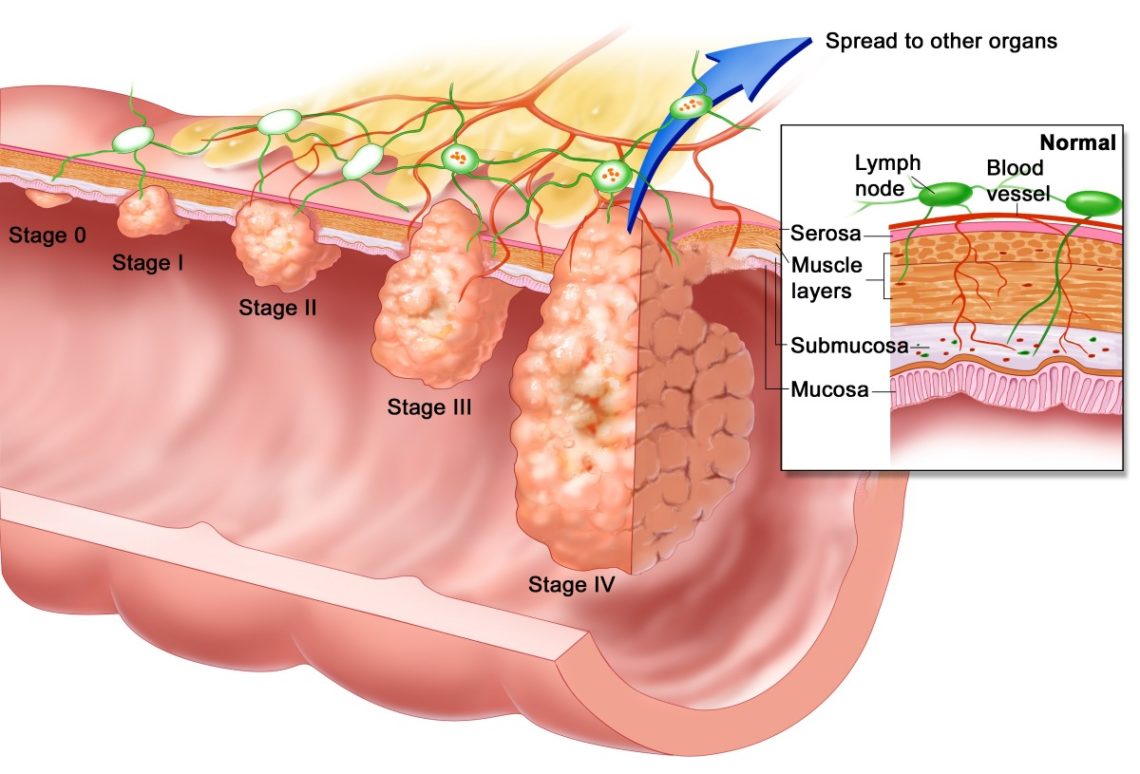
There are four stages / grades of piles.
There will be bleeding but no prolapse and can be seen only on proctoscopy
Findings: Hemorrhoids bulge into the lumen of the anal canal
Hemorrhoids may prolapse beyond the external sphincter and be visible during evacuation but reduce spontaneously.
Findings: Hemorrhoids bulge out of the anal canal during defecation but reduce all by themselves.
Hemorrhoids protrude outside the anal canal and require manual reduction.
Findings: Hemorrhoids bulge out of anus spontaneously or with defecation and require manual reduction.
Hemorrhoids are irreducible and are constantly prolapsed.
Findings: Hemorrhoids are irreducible and permanently prolapsed.
Four ways of treating piles.


Everything You Need To Know About Anal Fistula
Abnormal connection between the skin near anus & lining on the inside of anal canal is known as anal fistula.
Majority of anal fistulas are caused by abscesses that develop in the anal canal. As a result pus can drain onto the skin of its own or through an operation. Anal fistulas happen when the tract made by pus to the skin stays open.
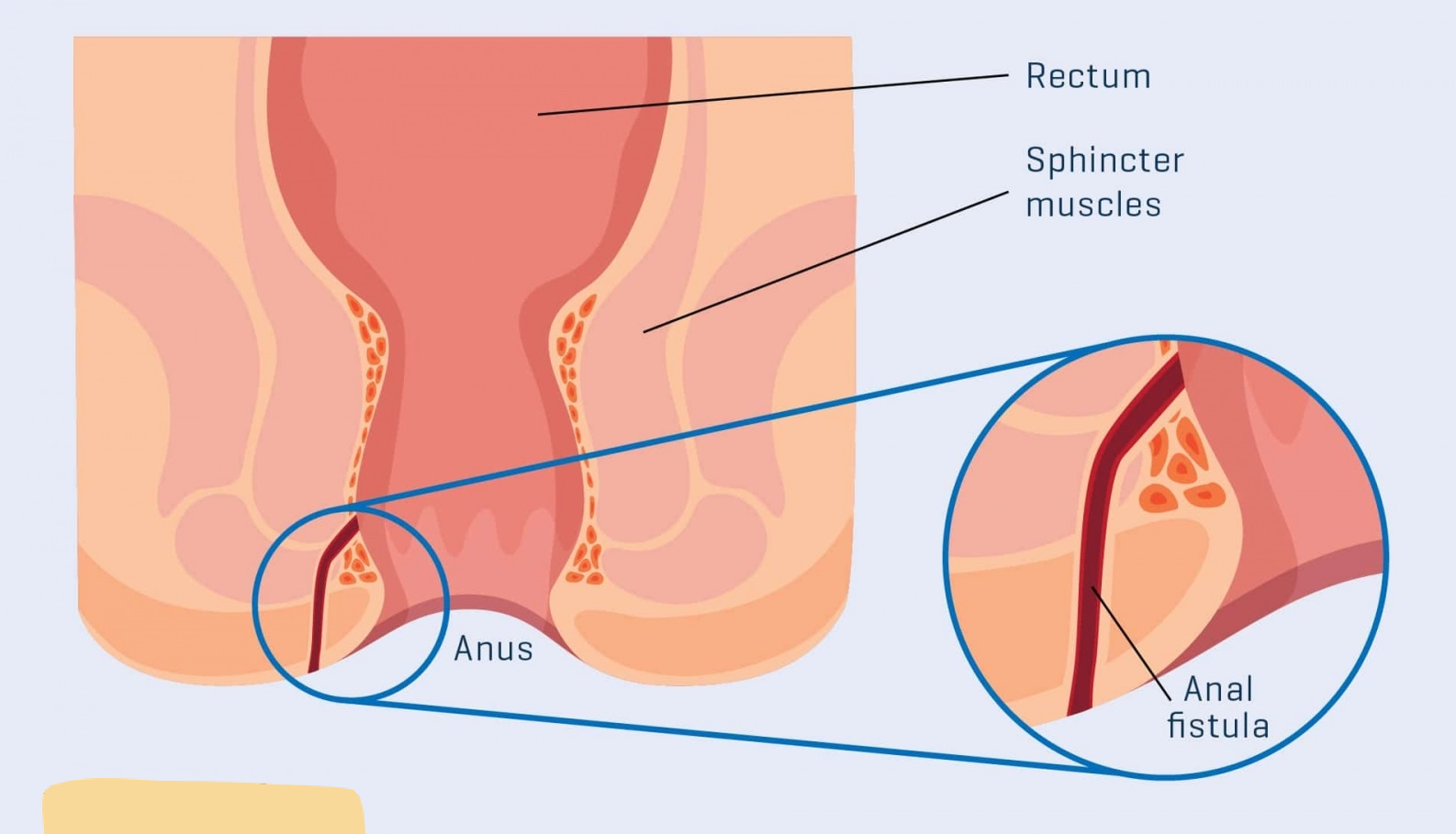
The leading causes of an anal fistula are clogged anal glands and anal abscesses.
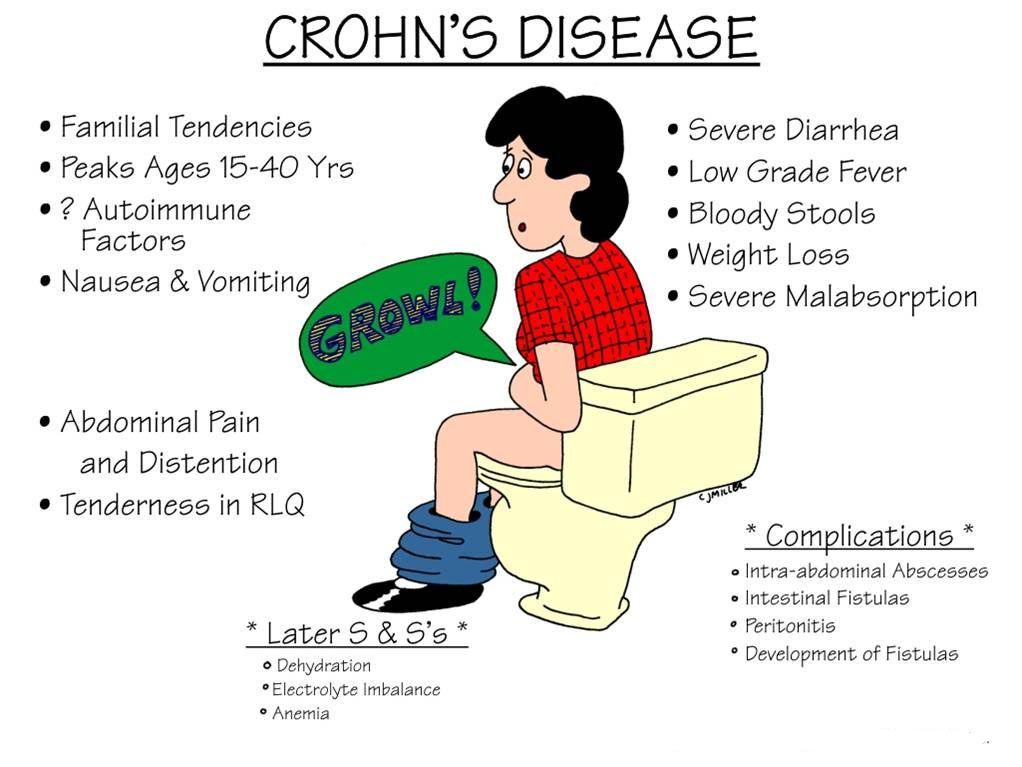
Other, much less common, conditions that can cause an anal fistula include:
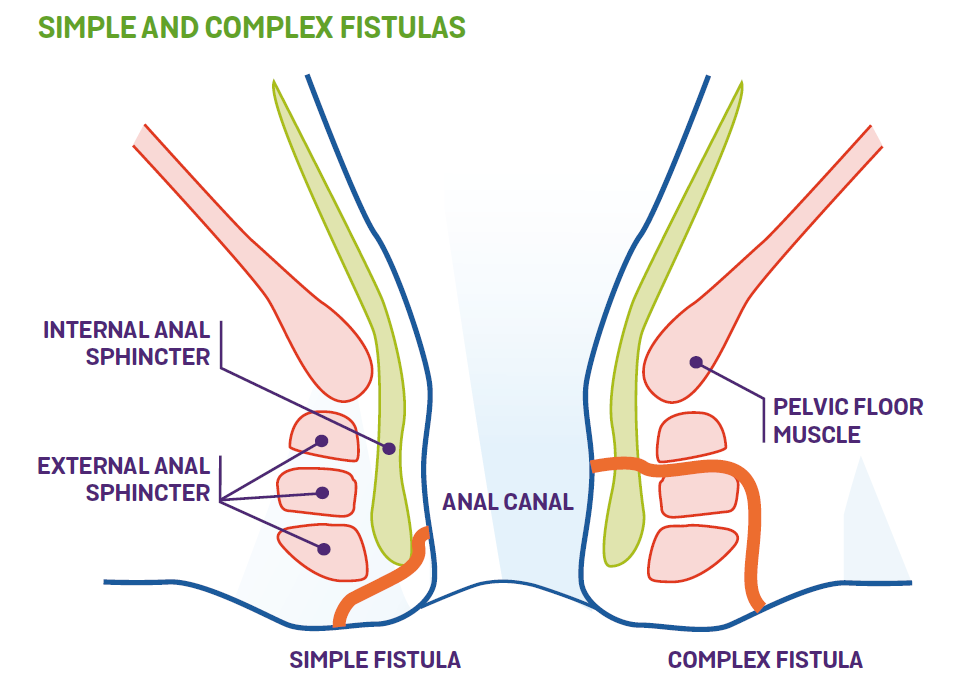
Different types of anal fistulas are classified by their location.
In order of most common to least common, the various types include:
The tract begins in the space between the internal and external sphincter muscles or in the space behind the anus. It then crosses the external sphincter and opens an inch or two outside the anal opening. These can wrap around the body in a U shape, with external openings on both sides of the anus (called a horseshoe fistula).
The tract begins in the space between the internal and external sphincter muscles and opens very close to the anal opening.
The tract begins in the space between the internal and external sphincter muscles and turns upward to a point above the puborectal muscle, crosses this muscle, then extends downward between the puborectal and levator ani muscle and opens an inch or two outside the anus.
The tract begins at the rectum or sigmoid colon and extends downward, passes through the levator ani muscle and opens around the anus. These fistulas are usually caused by an appendiceal abscess, diverticular abscess or Crohn's disease.
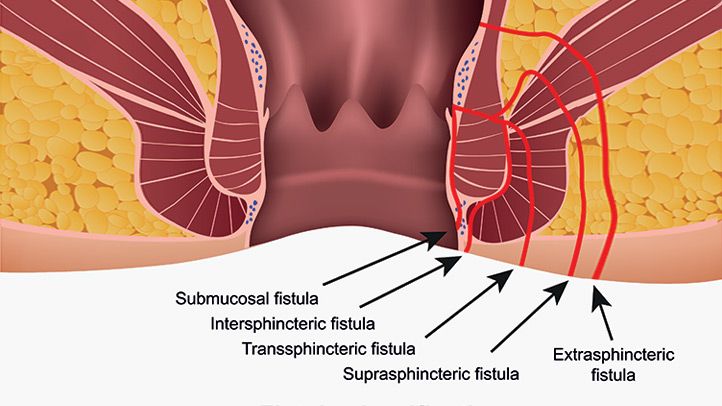

Treatment is delicately performed to reduce the risk of affecting bowel emptying, due to the anal fistulas' proximity to the anal sphincter muscles. The best approach requires that each patient is assessed individually. Treatment of an anal fistula is attempted with as little impact as possible on the sphincter muscles. It will often depend on the fistula's location and complexity, and the strength of the patient's sphincter muscles.
In a fistulotomy the surgeon first probes to find the fistula's internal opening. Then the tract is cut open and is scraped and its contents are flushed out, then its sides are stitch to the sides of the incision in order to lay open the fistula. A more complicated fistula, such as a horseshoe fistula (where the tract extends around both sides of the body and has external openings on both sides of the anus), is treated by usually laying open just the segment where the tracts join and the remainder of the tracts are removed. The surgery may be performed in more than one stage if a large amount of muscle must be cut. The surgery may need to be repeated if the entire tract can't be found.
A surgeon may core out the tract and then cut a flap into the rectal wall to access and remove the fistula's internal opening then stitches the flap back down. This is often done to reduce the amount of sphincter muscle to be cut.
A seton (silk string or rubber band) is used to either:
Create scar tissue around part of the sphincter muscle before cutting it with a knife
Allow the seton to slowly cut all the way through the muscle over the course of several weeks
The seton may also aid in the drainage of the fistula.
In some cases, fibrin glue, made from plasma protein, may be used to seal up and heal a fistula as opposed to cutting it open. The glue is injected through the external opening after clearing the tract and stitching the internal opening closed. A plug of collagen protein may also be used to seal and close the fistula tract.
It is usually simple to locate the external opening of an anal fistula, meanwhile locating the internal opening can be more challenging. It is important to be able to find the entire fistula for effective treatment.
People who may have experience with recurring anal abscesses may have an anal fistula . The external opening of the fistula is usually red, inflamed, oozes pus, and is sometimes mixed with blood. The location of the external opening gives a clue to a fistula's likely path and sometimes the fistula can actually be felt. However, locating its visual path often requires various tools, and often times it may not be seen until surgery.
Tools often used in diagnosis include:
Fistula probe. An instrument specially designed to be inserted through a fistula
Anoscope. A small instrument to view the anal canal
If a fistula is potentially complicated or in an unusual place, these tools may also be used:
Diluted methylene blue dye. Injected into a fistula
Fistulography. Injection of a contrast solution into a fistula and then X-raying it
Magnetic Resonance Imaging (MRI)
Tools used to rule out other disorders such as ulcerative colitis or Crohn's disease include:
Flexible sigmoidoscopy. A thin, flexible tube with a lighted camera inside the tip allows doctors to view the lining of the rectum and sigmoid colon as a magnified image on a television screen
Colonoscopy. Similar to sigmoidoscopy, but with the ability to examine the entire colon or large intestine
When recovering from anal fistula treatment, make sure to take pain medicine as directed by your surgeon. Finish all of your antibiotics. Don’t take any over-the-counter medicines without first talking to your provider.
Other important instructions may include:

Everything You Need To Know About Anal Fissure
Fissure is nothing but a small slit or tare in the anal region
An anal fissure is a tear or cuts in the thin lining of your anus that exposes the muscle around which is called the anal sphincter. The damage in the skin can often pull apart the edges of the fissure, cause the muscle to spasm, and make the condition worsen. Once the spasm occurs, the condition can be painful and the wound may take time to heal. Chronic diarrhea and constipation are bowel conditions that make anal fissures worse over time. Irrespective of age and gender, any individual can be at risk of developing an anal fissure. Although medical reports suggest that people between the age group of 20 to 40 are more at risk of getting anal fissures.
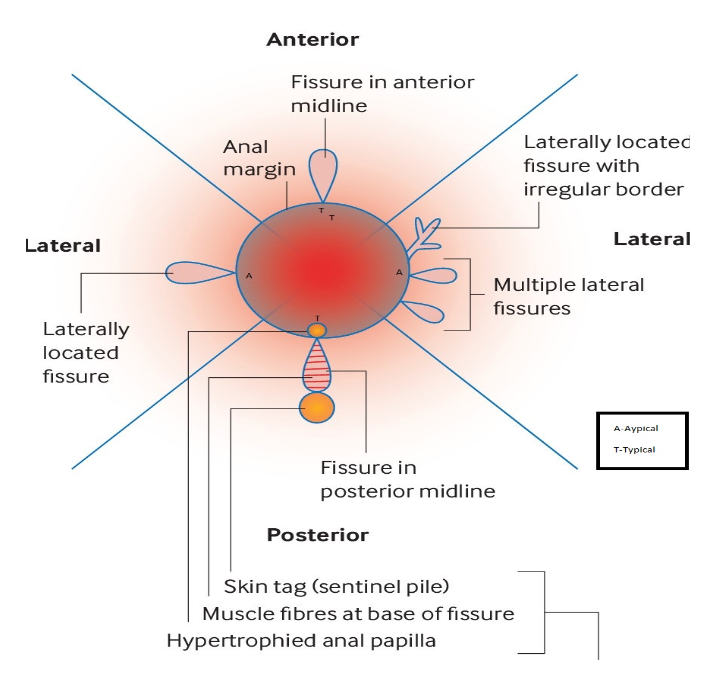
The anal fissure is caused by trauma to the anal canal and anus. Most people can remember during the bowel movement that their pain starts.
Common causes of the anal fissure such as:
Sexually transmitted Infections
Anal sex
Muscle spasms
Chronic constipation
Chances of contracting Crohn’s disease, Ulcerative Colitis, and other inflammatory bowel diseases in ulcers in the anal region.
Pregnancy and childbirth: during delivery, the line of the anus can tear and cause anal fissures.
Prolonged diarrhoea.
You may have these symptoms with an anal fissure:
Pain during and after a bowel movement
Visible tear or cut in the area
Bright red bleeding during or after a bowel movement

Your healthcare provider will make a diagnosis based on
Your personal health history
Your description of symptoms
Rectal exam
Because other conditions can cause symptoms similar to an anal fissure, your healthcare provider might also order tests to find out whether there is blood in your stool.

An acute anal fissure typically heals within 6 weeks with conservative treatment. Some disappear when constipation is treated. Anal fissures that last for 6 weeks or more are called chronic anal fissures. These fail conservative treatment and need a more aggressive, surgical approach.
People whose anal fissures don’t heal well may have an imbalance in anal pressure that prevents blood from circulating normally through the blood vessels around the anus. The reduced blood flow prevents healing. Medicine, Botox injections, and even some topical treatments that improve blood flow, may help anal fissures heal.People whose anal fissures don’t heal well may have an imbalance in anal pressure that prevents blood from circulating normally through the blood vessels around the anus. The reduced blood flow prevents healing. Medicine, Botox injections, and even some topical treatments that improve blood flow, may help anal fissures heal.
Other treatments include:
Changing your diet to increase fiber and water, steps that will help regulate your bowel movements and reduce both diarrhea and constipation
Taking warm baths for up to 20 minutes a day
Taking stool softeners, such as fiber supplements, as needed
Using topical medicines, such as nitrates or calcium blockers
Having surgery, such as a lateral internal sphincterectomy. During the surgery, the pressure inside the anus is released. This allows more blood to flow through the area to heal and protect tissues.
The risks from Botox injections and medicines used to treat anal fissures are relatively mild. Complications from surgery include the risk for infection, bleeding, and persistent gas and fecal incontinence, or uncontrolled bowel movements.

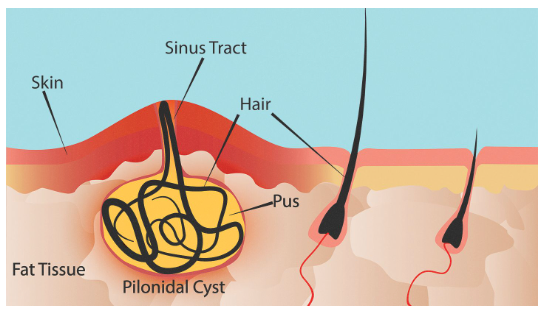
Everything You Need To Know About Pilonidal Sinus
A pilonidal sinus is a small tunnel that develops at the top of the crease in the buttocks. Trapped hair around the buttocks crease can lead to an abscess, and a pilonidal sinus may develop as a result.
If people have a pilonidal sinus, they may have discomfort and irritation around the tailbone area. In some cases, a pilonidal sinus may resolve by itself, but people may require treatment, such as abscess drainage or sinus removal.
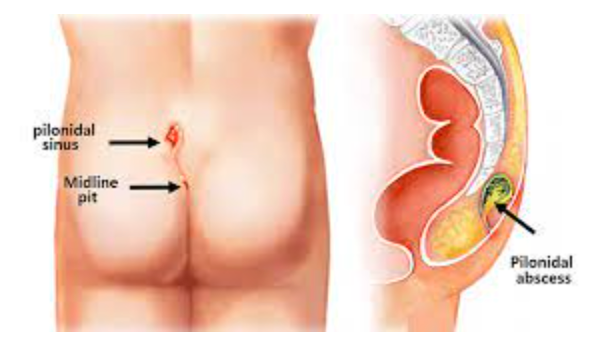
Pilonidal sinus is basically a skin problem. When there is too much friction and pressure in the anal area, the hair between the buttocks gets pushed inward.
This may either be caused by the hairs growing around the buttocks or due to the loose hair shed from the buttocks area that gathers around the cleft and gets into the pilonidal sinus.
Being male
Having a family history of pilonidal disease
Being overweight
Experiencing trauma or irritation in the area
Having a sedentary lifestyle or sitting down for long periods
Having a lot of hair around the buttocks
Practicing poor hygiene habits
Being younger, as pilonidal sinus is more common in young adults
Small dimple in the skin
Irritation or discomfort
Painful mass, which may be an abscess
Drainage from the area, which may be a clear, cloudy, or bloody fluid
Red, tender area
Foul-smelling pus
Fever, Nausea
If your case is diagnosed early on, you aren’t experiencing severe pain, and there’s no sign of inflammation, it’s likely that your doctor will prescribe a broad-spectrum antibiotic. A broad-spectrum antibiotic is an antibiotic that treats a wide range of bacteria. It’s important to realize that this won’t heal the sinus tract, but it will give you relief from the infection and discomfort. Your doctor will recommend that you get a follow-up exam, regularly remove hair or shave the site, and pay particular attention to hygiene.
This procedure alleviates symptoms from an abscess, or a collection of pus inside the sinus. Before this procedure, your doctor will give you a local anesthetic. They will then use a scalpel to open the abscess. They will clean away any hair, blood, and pus from inside the abscess.
Your doctor will pack the wound with sterile dressing and allow it to heal from the inside out. The wound usually heals within four weeks, and many people don’t require any further treatment.
For this type of treatment, your doctor will first give you a local anesthetic. They will then inject phenol, a chemical compound used as an antiseptic, into the cyst. This procedure may need to be repeated several times. Eventually, this treatment will cause the lesion to harden and close.
This treatment has a very high recurrence rate. Therefore, it’s uncommon. Doctors turn to surgery as the treatment of choice in some cases.
If you have a recurring Pilonidal Sinus or if you have more than one sinus tract, your doctor will recommend a surgical procedure.
You will first be given a local anesthetic. Then, the surgeon will open the lesions, removing all of the pus and debris. Once this process is complete, the surgeon will stitch the wounds closed.
After surgery, your doctor will explain how to change the dressings and will recommend shaving the site to prevent hair from growing into the wound.
There are four stages / grades of piles.
There will be bleeding but no prolapse and can be seen only on proctoscopy
Findings: Hemorrhoids bulge into the lumen of the anal canal
Hemorrhoids may prolapse beyond the external sphincter and be visible during evacuation but reduce spontaneously.
Findings: Hemorrhoids bulge out of the anal canal during defecation but reduce all by themselves.
Hemorrhoids protrude outside the anal canal and require manual reduction.
Findings: Hemorrhoids bulge out of anus spontaneously or with defecation and require manual reduction.
Hemorrhoids are irreducible and are constantly prolapsed.
Findings: Hemorrhoids are irreducible and permanently prolapsed.
Four ways of treating piles.


Our experts are here for you every single day! We care about our patients and we do our best to make them happy.

2nd Generational professional skilled in anorectal surgeon with 13 years of experience treating 10000+ acute & chronic cases in the field of proctolgy.
+91 9886933258
Has great experience Proctologist. Persisting with 6 years of experience in ano rectal disorders.
+91 9902105857
Dr Poonam is a renowned proctologist, who majorly deals with all sorts of Anorectal disorders. Such as Hemorrhoids ( Piles ) , Fistula and Fissures. With 6 years of experience.

Dr Shagufta Banu is a renowned proctologist, she has an tremendous experience of more than 12 years and she has been treated more than 15,000+ patients in her career.

An authentic with a traditional surgical skills and experienced of 3 years in field of Proctolgy
+91 8904402320The laser piles surgery is a non-invasive procedure done on an outpatient basis and takes only about 30 to 45 minutes to complete.
Yes. You can book both online and offline consultation with our doctors without any hassle. Just fill the appointment form available on the website and we’ll get back to you to schedule an appointment at your convenience.
Grade I- Small inflammations inside the anal lining which are not visible to the eyes.
Grade III- Also known as prolapsed piles as the veins hang out of the anus. These can be re-inserted manually.
Grade IV- These are large inflammations that remain hanging out of the anus and require surgery as treatment.
If you are suffering from Piles and are searching for a ‘piles specialist near me’, then opting for piles surgery is the safest and quickest remedy. Approximately, the cost of Piles surgery in bangalore is starting from INR 35,000 only. However, the cost depends on a number of factors. To know how much piles surgery will exactly cost you, contact the Shifa Piles Clinic support team.
Surgery is the best procedure for Piles treatment. However, your doctor can also recommend non-surgical procedures like sclerotherapy, banding and coagulation depending on your condition. A doctor may also prescribe you medication to treat the ailment.

Whitefield, Bengaluru, Karnataka
Shifa Piles Clinic Bus stop, Z P Complex Entrance, Nagondanahalli Main Rd, near Whitefield, Bengaluru, Karnataka - 5600662
shifapilescare@gmail.com
+91 9886933258
+91 9902105857
+91 8904402320